The Hindu: Mumbai: Sunday, June 03, 2018.
Officials say
tighter regulations the cause; activists say no watertight system of monitoring
in place
There is a
gradual revival in the number of clinical trials being done in India. From an
all time low of 17 clinical trials approved by the Drug Controller General of
India (DCGI) in 2013, the number has slowly increased to 97 in 2017, a more
than 400% jump in five years.
Regulators
and domain experts attribute the revival to introduction of scientific and
balanced guidelines that suit all stakeholders. Activists, however, feel India
is far from a watertight system when it comes to monitoring the trials.
But the jump
in numbers is nowhere close to the pre-2013 period. For example, in 2012, the
DCGI approved 253 trials, in 2011, the number stood at 283 and in 2010 at 529.
“We are seeing some parity being restored,” said Suneela Thatte, board member
of the Indian Society of Clinical Research, a clinical research professionals’
association.
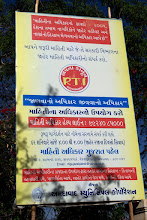
In February
2012, a PIL plea filed by the Swasthya Adhikar Manch in the Supreme Court
raised an alert over many irregularities in clinical trials, including lack of
consent and compensation to the patients referred to as subjects. Around the
same time, the 59th Parliamentary Committee report stated that there was a
strong nexus between drug makers, doctors and some government regulators. In
January 2013, a gazette notification by the Ministry of Health and Family
Welfare determining the eligibility for compensation eventually led to many
drug makers hunting for other locations for trials. “The clause of compensation
was open to misuse and could act as an inducement for participation in the
trial as it called for free medical management in terms of injury to the
clinical trial subject. There was no distinction made between study related
injury or non-related injury,” said Ms. Thatte, adding that approval time of
clinical trials would also take extremely long.
According to
DCGI Dr. S. Eswara Reddy there were many other clauses that were brought in:
like investigators could not undertake more than three trials, to be conducted
only in government hospitals, the site of trials should be 50-bed hospitals,
etc. “Gradually, we have begun harmonizing the clinical trial environment as
per international standards,” Dr. Reddy told The Hindu, adding that now 50% of
the trials can be conducted in private hospitals, there is no restriction of
three trials per investigator and a formula for calculating financial
compensation has been derived.
Genuine
subjects?
However, the
recent case of a clinical trial in Jaipur mired in a controversy where patients
were allegedly deceived into participating in the trial. “The incident exposes
the loopholes in government regulations,” said Amulya Nidhi, co-convenor of
Swasthya Adhikar Manch. “Indians continue to be guinea pigs”, he said.
According to
the Health Ministry, there were 436 serious adverse events (SAE) of deaths in
clinical trials in 2012, 590 in 2013 and 443 in 2014. Of these, 16, 46 and 22
respectively were established to be related to clinical trials. In 2015 there
were 162 deaths but data on those established due to clinical trials was
unavailable. “If you check the government data, it will show many people were
given compensation. But we keep asking them for the names of addresses which
they refuse,” said Mr. Nidhi, adding that there are no drug inspectors for
regular checks on trials and private hospitals don’t come under the Right To
Information (RTI) Act. “No one knows what is exactly happening on the ground level.
Violations continue to happen,” he said.